Connect With Us!
If you’re considering osseointegration, or you’ve completed your surgery and are now enjoying life with osseointegration, we want to hear from you! Share your ideas, news, stories, feedback and pictures with us here!
Socket prosthetics have long been a standard solution for upper and lower limb amputees. Since the first human surgery in 1965, osseointegration, the use of a bone-anchored implant to secure an external prosthetic, has emerged as a favourable alternative to the use of socket prosthetics for people living with limb loss.
While many healthcare providers continue to rely on socket technology as a first-choice therapy for amputees, year-on-year the number of surgeons performing osseointegration, and the number of people with limb loss receiving osseointegrated implants, continues to grow.
Below you will find up-to-date research which details the benefits of osseointegration for amputees struggling with traditional socket prosthetics, as well as the complications that are known to occur with osseointegration, and other information that you may find useful.
Compared with traditional socket-based prosthetics, osseointegrated prosthetics have been shown to confer a range of benefits.
Skin problems such as lesion and cyst development, infection, ulceration, blistering, sensitivity and breakdown are common complications associated with the use of socket prosthetics [1, 2, 3, 4]. Uneven loading within the socket can result in skin pulling and rubbing [1]; contact dermatitis can be caused by the materials from which the socket prosthetic itself is made [1,6]. The nature and prevalence of these complications is influenced by a wide range of individual factors, including the level of amputation.
In fact, in one study, socket-related skin problems were reported by more than 70% of participants [5]. Other studies have reported that up to 60% of people with limb loss report dissatisfaction with their socket prosthetic, and almost one third reject the socket prosthetic altogether [7], thus dramatically reducing their mobility and daily activity levels [8].
Because osseointegration offers a stable, direct connection between the bone and the implant, the soft tissue of the residual limb is no longer subject to the pressure, pulling or excessive heating and sweating caused by the socket or by size and shape variation over time in the residual limb [9]. Minor skin irritation can occur at the interface between the skin and the implant for a period following surgery, although this typically resolves with time [10].
Traditional above-knee or transfemoral socket prosthetics of all types significantly restrict hip range of motion (ROM). Ischial Containment Sockets (ICS), particularly, prevent normal physiological movement by enclosing the ischial tuberosity and ramus, but sockets of all types have been shown to cause restrictions of both hip abduction and extension [11, 14].
Studies comparing socket prosthetic users with osseointegrated individuals demonstrate no restriction of hip range of motion with osseintegration [12]. Indeed, one study of patients who had previously relied on a traditional socket prosthetic and subsequently received an osseointegrated implant demonstrated that osseointegration allows people with above-knee amputation to significantly increase their hip extension and reduce pelvic tilt, achieving a gait pattern comparable to non-amputated controls [13].
Socket prosthetics have been shown to significantly reduce walking speed and to have a negative effect on other mobility parameters, including stability and confidence [15, 16, 17].
The Timed Up and Go (TUG) test can be used to measure physical mobility, assess the risk of falls and predict prosthetic non-use in prosthetic-wearing patients with lower-limb amputation. It requires a patient to stand up from a chair, walk to a point three metres distant from the chair, turn around, walk back to the chair, and sit [19].
Recent work has demonstrated that, on average, osseointegrated patients completed the test almost 20% faster than those using socket prosthetics and achieved a mean test time value comparable to those of unamputated controls.[20] Studies utilising the 6-Minute Walk Test (6MWT), which measure how far a person can walk in 6-minutes, have shown that shown that osseointegrated patients can walk approximately 25% further and with greater ease (measured by the total amount of oxygen used during walking) than those using socket prostheses [21].
Osseointegration has also been shown to improve balance and walking confidence among transfemoral amputees [18]. This also results in greater socket use, and by extension, a higher level of movement and activity for osseointegrated individuals [21, 22].
Unlike socket prosthetics, osseointegration restores the normal position of the bone within the residual limb and aligns it along its correct physiological axis (see figure) [23]. Proper alignment and resulting good posture can help to prevent the development of painful or degenerative musculoskeletal problems.
 For people with unilatera lower limb loss, socket prosthetic use is associated with uneven loading onto the intact limb which can cause hip and knee osteoarthritis [24]. Disuse osteopenia is another common problem among people with lower limb loss. It is characterised by low bone density resulting from poor loading through the residual bone, and can cause pain in the lower back and hips.
For people with unilatera lower limb loss, socket prosthetic use is associated with uneven loading onto the intact limb which can cause hip and knee osteoarthritis [24]. Disuse osteopenia is another common problem among people with lower limb loss. It is characterised by low bone density resulting from poor loading through the residual bone, and can cause pain in the lower back and hips.
Recent study has demonstrated that osseointegration can reduce bone loss in both the lumbar spine and parts of the femur between one and two years after surgery. This effect is illustrated in the graph below, which depicts bone density z-scores for the lumbar spine in different patient categories:
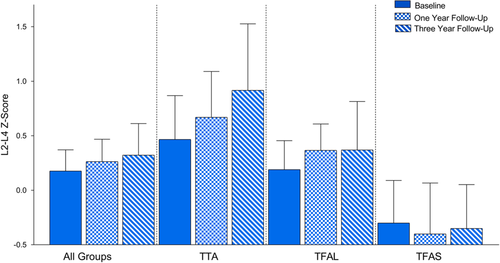
Note: TTA = Trantibial amputee; TFAL = Transfemoral amputee with long residual femurs; TFAS = Transfemoral amputee with short femurs requiring a metallic screw in the femoral neck.
Research has demonstrated that osseointegrated amputees experience tactile sensations through their implant which can involve sensory receptors in the muscles, joints and soft tissue, and which can be accompanied by new changes in the ways your brain processes these stimuli. [25]
This ability is known as osseoperception and allows those living with limb loss to experience changes in the topography and materiality of the surface that they’re walking on, as well as environmental changes like wind strength, through their prosthetic limb.
As well as tactile stimuli, sound frequencies are also perceived through the osseointegrated implant, making osseoperception a ‘multi-sensory’ phenomenon and helping to explain this improved environmental perception. [26]
Health-related quality of life for those living with limb loss is typically measured with reference to a range of different components of everyday life using a number of different scales (e.g., LIFE-H, SF-36 and Q-TFA). [27]
Multiple studies have shown osseointegration to be associated with often significant improvements in self-reported health-related quality of life scores at follow-up. Scales have included components such as recreation, mobility, fitness and personal care, as well as measures for mental health and wellbeing. [28]
All surgeries carry a degree of risk and uncertainty around their long-term outcomes. While osseointegration has been shown to be a safe and effective therapeutic option, some patients may experience complications following their surgery.
These range from more common, easily treatable complications such as superficial infection, to more significant complications, like periprosthetic fracture or implant failure. The following list highlights some of the potential complications associated with osseointegration surgery.
Superficial infection is a relatively common experience among osseointegration patients. Good hygiene is key to minimising the risk of infection. Typically, superficial infections affect around a third of all osseointegration patients and can be successfully treated by a short course of antibiotics.
Less commonly, patients may contract an infection which affects the deeper layers of the soft tissue or the bone. In this case, it may be necessary to remove the implant and clear the infection before refitting the implant.[29] For patients living in tropical or subtropical climates, good hygiene is important in keeping insects clear of the stoma and preventing Myiasis.
If the implant fails to bond with the bone, or is overloaded, or if the bone becomes infected, there is a risk that the implant could loosen. If this occurs, it will typically be necessary to remove the implant and refit it.
Injuries of this type are known to occur during osseointegration surgery. They can result in discomfort or numbness in the affected area.
Force applied to the bone during implantation can place additional stress on the bone. Periprosthetic fractures – those occurring in the area of the osseointegrated implant – are rare, occurring in around 4% of osseointegrated patients, typically following a fall and normally in the femur. Research has shown that females are at increased risk of sustaining a periprosthetic fracture (3.89-fold increased risk), as are those of heavier weight (1.02-fold increase per kg above a bodyweight of 80.4kg) [30].
Treatment normally involves fixation of the fracture, but doesn’t require the implant to be removed and, for most, doesn’t impact long-term osseointegrated prosthetic use [30].
Although osseointegration mitigates many of the skin complaints associated with the use of socket-mounted prosthetics, it is still possible for osseointegrated patients to experience some skin irritation at the interface between the soft tissue and the percutaneous portion of the implant.
Patients with malnutrition, or with vascular deficits in the affected limb, may also experience delayed healing of the surgical site.
It is perfectly normal to experience some pain around the surgical site following osseointegration surgery. This is normally controlled with prescription painkilling medication.
If osseointegration is undertaken at the same time as amputation, then the patient may experience phantom limb pain. This can often be mitigated or minimised by undertaking Targeted Muscle Reinnervation (TMR) or Regenerative Peripheral Nerve Interfaces (RPNI), which redirects the nerves cut during the amputation and enables them to continue to receive signals and thereby function as they would otherwise have done. [31, 32].
Some people undergoing osseointegration may also develop highly sensitive nerve bundles called neuromas. Neuroma pain too has been shown to be significantly reduced by RPNI/TMR, which may even prevent neuromas from forming in the first place [33, 34].
The numbered references referred to above are listed below, should you wish to carry out your own research.
[1] Belovs, L. and Lannan, F.M. (2024) Dermatologic conditions in persons with lower limb amputations: a review. Current physical medicine and rehabilitation reports, 12(1), 11–18. Available at: https://doi.org/10.1007/s40141-023-00427-1.
[2] Pezzin, L.E. et al. (2004) Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil, 85, 723–729.
[3] Dillingham, T.R. et al. (2001) Use and satisfaction with prosthetic devices among persons with trauma-related amputations. American Journal of Physical Medicine & Rehabilitation, 80(8), 563–571. Available at: https://doi.org/10.1097/00002060-200108000-00003.
[4] Lyon, C.C. et al. (2000) Skin disorders in amputees. Journal of the American Academy of Dermatology, 42(3), 501–507. Available at: https://doi.org/10.1016/s0190-9622(00)90227-5.
[5] Colgecen, E., et al. (2016). A clinical evaluation of skin disorders of lower limb amputation sites. Int J Dermatol. 55(4), 468–472.
[6] Munoz, C.A., Gaspari, A. and Goldner, R. (2008) Contact dermatitis from a prosthesis. Dermatitis, 19(2),109-11.
[7] Baars, E.C., Schrier, E., Dijkstra, P.U. and Geertzen, J.H.B. (2018) Prosthesis satisfaction in lower limb amputees: a systematic review of associated factors and questionnaires. Medicine (Baltimore), 97(39), e12296. Available at: https://doi.org/10.1097/MD.0000000000012296
[8] Ontario Health (Quality) (2019) Osseointegrated prosthetic implants for people with lower-limb amputation: a health technology assessment. Ont Health Technol Assess Ser [Internet], 19(7),1-126.
[9] Overmann, A.L. and Forsberg, J.A. (2020) The state of the art of osseointegration for limb prosthesis. Biomed. Eng. Lett. 10, 5–16. Available at: https://doi.org/10.1007/s13534-019-00133-9.
[10] Hoellwarth, J.S. et al. (2021) Transcutaneous osseointegration for amputees. Lessons from the past of relevance to the future. Bone Joint Res.,10(10):690–692.
[11] Klotz, R., Colobert, B., Botino, M., and Permentiers, I. (2011) Influence of different types of sockets on the range of motion of the hip joint by the transfemoral amputee. Ann Phys Rehabil Med. 54(7), 399-410. Available at: https://doi.org/10.1016/j.rehab.2011.08.001
[12] Hagberg, K. et al. (2005) Socket versus bone-anchored trans-femoral prostheses. Prosthetics & Orthotics International, 29(2), 153–163. Available at: https://doi.org/10.1080/03093640500238014
[13] Tranberg, R., Zügner, R., and Kärrholm, J. (2011) Improvements in hip and pelvic motion for patients with osseointegrated trans-femoral prostheses. Gait Posture 33, 165–168.
[14] Gaunaurd, I., et al. (2011) Postural asymmetries in transfemoral amputees. Prosthetics and Orthotics International 35(2), 171-180
[15] Gailey, R. et al. (2010) Unilateral lower-limb loss: prosthetic device use and functional outcomes in servicemembers from Vietnam war and OIF/OEF conflicts. J Rehabil Res Dev. 47(4), 317-31.
[16] Roffman, C.E., Buchanan, J. and Allison, G.T. (2014) Predictors of non-use of prostheses by people with lower limb amputation after discharge from rehabilitation: development and validation of clinical prediction rules. Journal of Physiotherapy,
60(4), 224-231.
[17] Turner, S., Belsi, A., and McGregor, A.H. (2022) Issues faced by people with amputation(s) during lower limb prosthetic rehabilitation: a thematic analysis. Prosthet Orthot Int. 46(1), 61-67.
[18] Gaffnet, B.M.M. et al. (2023) Osseointegrated prostheses improve balance and balance confidence in individuals with unilateral transfemoral limb loss. Gait & Posture 100, 132-138.
[19] Schoppen, T., et al. (1999) The timed “up and go” test: reliability and validity in persons with unilateral lower limb amputation. Arch Phys Med Rehabil 80, 825-828.
[20] Al Muderis, M. et al. (2024) Transtibial osseointegration following unilateral traumatic amputation: An observational study of patients with at least two years follow up. Injury 55, 111568.
[21] Van de Meent, H., Hopman, M.T. and Frölke, J.P. (2013) Walking ability and quality of life in subjects with transfemoral amputation: a comparison of osseointegration with socket prostheses. Archives of Physical Medicine and Rehabilitation, 94(11), 2174–78. Available at: https://doi.org/10.1016/j.apmr.2013.05.020
[22] Hoellwarth, J.S., Tetsworth, K., Rozbruch, S.R., Handal, M.B., Coughlan, A., and Al Muderis, M. (2020) Osseointegration for amputees: current implants, techniques, and future directions. JBJS Rev. 8(3), e0043. Available at: https://doi.org/10.2106/JBJS.RVW.19.00043
[23] Thomson, S. et al. (2019) Proximal bone remodelling in lower limb amputees reconstructed with an osseointegrated prosthesis. Journal of Orthopaedic Research, 37(12), 2524–2530. Available at: https://doi.org/10.1002/jor.24445.
[24] Wade, L., McGuigan, M.P., McKay, C., Bilzon, J. and Seminati, E. (2022) Biomechanical risk factors for knee osteoarthritis and lower back pain in lower limb amputees: protocol for a systematic review. BMJ Open. 12(11):e066959. Available at https://doi.org/10.1136/bmjopen-2022-066959
[25] Hagberg, K., Häggström, E., Jönsson, S., Rydevik, B. and Brånemark, R. (2008). Osseoperception and Osseointegrated Prosthetic Limbs, in Gallagher, P., Desmond, D., MacLachlan, M. (eds) Psychoprosthetics. Springer, London. Available at: https://doi.org/10.1007/978-1-84628-980-4_10
[26] Clemente, F. et al. (2017). Touch and hearing mediate osseoperception. Scientific Reports 7, 45363. Available at: https://doi.org/10.1038/srep45363
[27] Kunutsor, S.K., Gillatt, D. and Blom, A.W. (2018) Systematic review of the safety and efficacy of osseointegration prosthesis after limb amputation, British Journal of Surgery 105(13), 1731–1741. Available at: https://doi.org/10.1002/bjs.11005
[28] Handford, C., McMenemy, L., Kendrew, J., Mistlin, A., Akhtar, M.A., Parry, M. and Hindle, P. (2022) Improving outcomes for amputees: the health-related quality of life and cost utility analysis of osseointegration prosthetics in transfemoral amputees, Injury, 53 (12), 4114-4122. Available at: https://doi.org/10.1016/j.injury.2022.10.007
[29] Al Muderis, M., Khemka, A., Lord, S.J., Van de Meent, H. and Frölke, J.P.M. (2016) Safety of osseointegrated implants for transfemoral amputees: a two-center prospective cohort study. J Bone Joint Surg Am 98(11), 900-09. Available at: https://doi.org/10.2106/JBJS.15.00808
[30] Hoellwarth, J.S, Tetsworth, K., Kendrew, J., Kang, N.V., van Waes, O., Al-Maawi, Q., Roberts, C. and Al Muderis, M. (2020) Periprosthetic osseointegration fractures are infrequent and management is familiar. Bone Joint J. 102-B(2):162-169.
[31] Valerio, I.L. et al. (2019) Pre-emptive treatment of phantom and residual limb pain with Targeted Muscle Reinnervation at the time of major limb amputation, J. Am. Coll. Surg. 228(3), 217–226.
[32] Tropf, J.G. and Potter, B.K. (2023) Osseointegration for amputees: current state of direct skeletal attachment of prostheses. Orthoplastic Surgery 12, 20-28.
[33] Kubiak, C.A. et al. (2022) Decreasing postamputation pain with the Regenerative Peripheral Nerve Interface (RPNI). Annals of Vascular Surgery 79, 421-426.
[34] Vernice, N.A. et al. (2022) Osseointegration for lower-extremity amputees: operative considerations from the plastic surgeon’s perspective. JBJS Rev. 10(11), e22.00125. Available at https://doi.org/10.2106/JBJS.RVW.22.00125
If you’re considering osseointegration, or you’ve completed your surgery and are now enjoying life with osseointegration, we want to hear from you! Share your ideas, news, stories, feedback and pictures with us here!

The Osseointegration Group exists to enable amputees worldwide to improve their quality of life through the application of clincal expertise and technical and technological innovation.
The OPL Device is not approved for sale in the US. Please contact us for further information on device availability in your region. Information provided via this website is for educational and communication purposes only. The material presented represents techniques and procedures used by The Osseointegration Group (OG). OG disclaims any and all liability for injury and/or other damages which result from an individual using techniques presented on this website.