An osseointegrated (bone-anchored) implant eliminates the need for a prosthetic socket, eliminating socket-related pain and irritation while providing improved mobility, comfort and quality of life.
Vision
The result of decades of innovation, and the very latest in technique and technology, osseointegration offers a real alternative to traditional sockets that have helped transform the lives of over 1500 patients to date.
Patient Share how osseointegration restored their confidence and mobility
Direct Skeletal attachment creates a natural connection your body recognize.
Understand how osseointegration can transform your quality of life
Eliminate rubbing, chafing, pressure pain and skin breakdown.
Sitting, walking or running, say goodbye to the daily pains associated with socket use.
Enjoy lower energy consumption and less fatigue compared to socket prostheses, leaving you with the power to do more!
Experience your environment with improved proprioception, from walking surfaces to wind.
Be confident in your movement, with better muscle strength and a more natural gait.
With a customised fit, you can enjoy perfect height and alignment for your prosthetic.

With an antimicrobial coating, a microporous surface designed to optimise bone growth and over 159 sizes to ensure a perfect fit every time, it’s no wonder that OPL is a first choice
...
Patients benefit from attachment and removal in as little as ten seconds, as well as a host of safety features which protect against falls and twisting.
Compatible with most prosthetic limbs, the OPL is suitable for above- and below-knee limb loss, hip disarticulation, and digital and upper limb loss, and is fitted during a single-stage surgery for a rapid return to mobility and an optimised recovery.
Lives transformed by osseointegration
I walk without thinking about my prosthetic anymore. It feels like part of me again.
The pain stopped. The confidence came back. Everything changed in ways I didn't expect.
I can wear my prosthetic all day now without the skin breakdown I used to dread.
Country
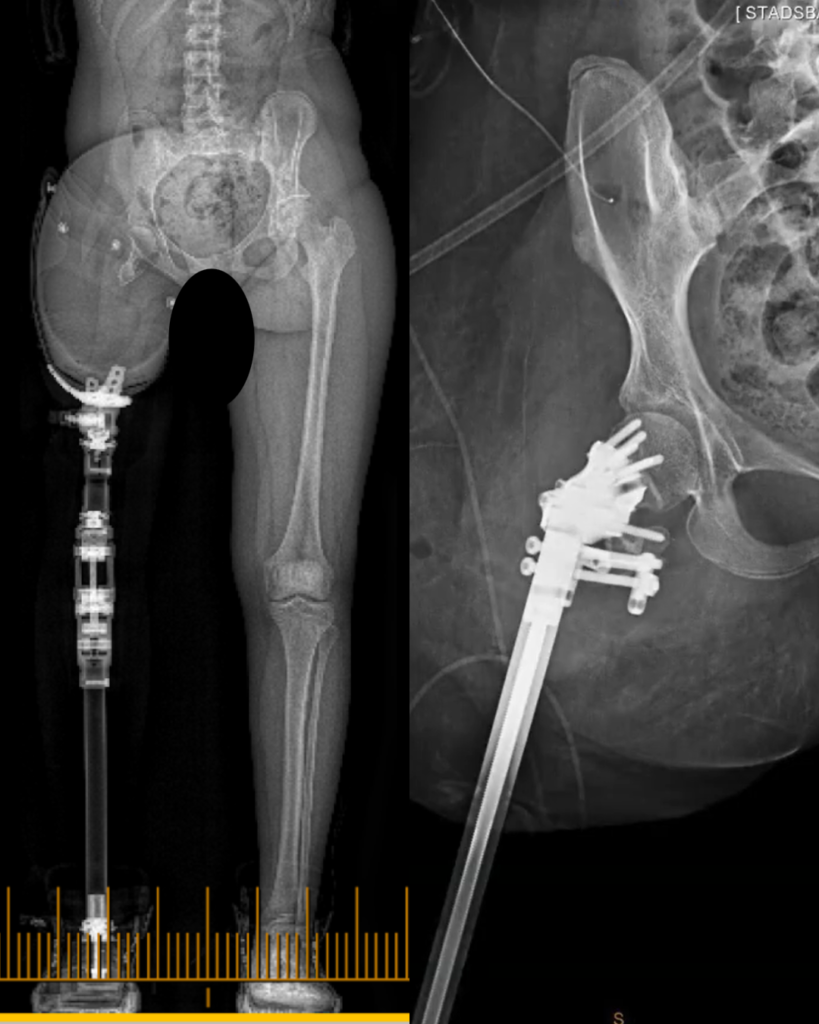
Belgium
Condition
Ewing’s Sarcoma
Challenge
extremely short residual femur (21.7mm)
Solution
lengthening + osseointegration + custom implant.
Country
Australia
Condition
Bilateral amputation
Challenge
Knee arthritis made implant load unbearable
Solution
BK OPL customised to attach to baseplate of TKR.

Country
Australia
Condition
CRPS
Danger of CRPS spreading
Solution
Unilateral amputation + Osseointegration + Nerve surgery.

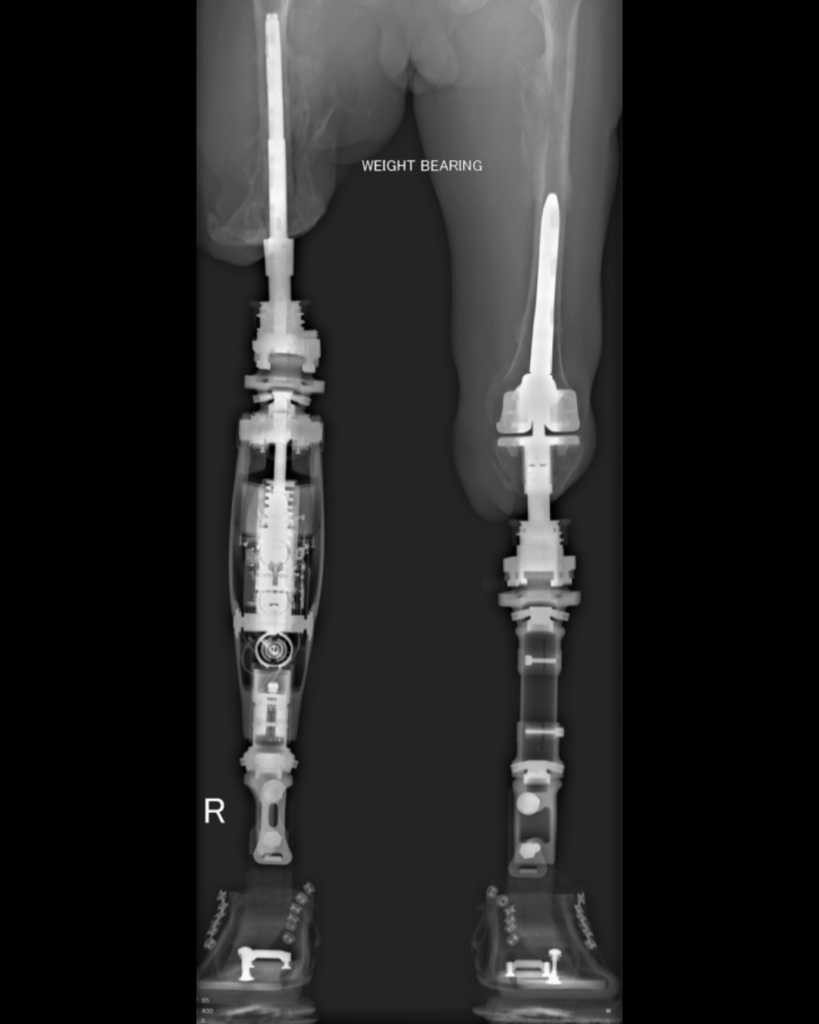
Country
Australia
Condition
Persistent infection, fractures, complicated by malnutrition + severe osteoporosis
Solution
Bilateral amputation + Osseointegration + Intensive physiotherapy.

Country
United States
Condition
Very short residuum following amputation
Solution
Above-knee OPL osseointegration.

Country
Italy
Condition
Right transfemoral amputation
Solution
Above-knee OPL osseointegration.
Confidential and secure. Response within 24 hours.
A member of our clinical management team will contact you to discuss your enquiry in more detail, and answer any questions you may have.
We’re working hard to ensure that world leading osseointegration care is available globally. We currently operate clinics in Florida, US; Abu Dhabi, UAE and Sydney, Australia, and can deliver care at other clinics across Europe and Asia.
If you are a healthcare professional interested in bringing osseointegration to your region, please get in touch with our clinical team.
Paley Orthopedic & Spine Institute
901 45th Street
Kimmel Building, West Palm Beach, FL 33407
Suite 303, Level 3, 2 Technology Place,
Macquarie University NSW 2220, Australia.
Burjeel Medical City
28th Street - Mohamed Bin Zayed City - Z9 - Abu Dhabi - United Arab Emirates
If you’ve ever had a question about osseointegration, it’s likely that someone else has too.
Check out some general answers to questions we’ve received below, including those related to cost, candidate suitability, aftercare and more.
Most patients will require only one single stage surgery to fit the implant. For more complex cases, where it is in the patient’s best interest, the decision may be taken to complete osseointegration over two stages, separated by a period of months. Patients with very short residual limbs may also require lengthening prior to osseointegration.
Even during single stage surgery, it is often possible to complete additional procedures alongside the fitting of the implant, which are designed to improve patient outcomes.
Osseointegration is suitable for people with upper and lower limb loss, as well as those who have lost fingers to amputation, even where the residual bone is very short.
For the lower limb, osseointegration is possible for:
For the upper limb, osseointegration is possible for:
Osseointegration Group is also the only team experienced in complex osseointegration at the shoulder (scapula) or hip (pelvic) for people with whole limb loss.
For people who have been unable to benefit from other types of treatment, and where the limb is not salvageable, amputation with subsequent osseointegration may be a viable therapeutic option.
Where this may be the case, you will be invited to complete individual assessments with members of our multidisciplinary team, including a pain specialist, psychologist, prosthetist and physiotherapist, to ensure that amputation is the right choice for you.
In short, no.
No two osseointegration procedures are the same, because no two patients are the same; varying as they do in the nature and level of their amputation, the time since amputation, the quality of their bone, the presence or absence of additional health issues and, of course, their individual needs.
Accounting for these individual factors also means that the costs associated with osseointegration can vary from patient to patient.
Conditions like insulin-dependent diabetes can negatively impact the healing process. For this reason, patients with diabetes can be at higher risk of implant failure.
However, recent advances in surgical technique and technology mean that patients with well-controlled diabetes are now able to undergo osseointegration.
No. Antibiotics are a key part of our post-operative infection reduction protocol, but are not typically used in the longer term for patients without a history of recurrent infection.
Yes, absolutely!
Once your wound has healed and you have received the go-ahead from your surgeon, you are encouraged to swim in the ocean as the saltwater will help with the healing process. You should avoid freshwater (rivers, lakes and pools) and chlorinated public swimming pools for around a year after your surgery, due to the much higher risk of infection.
When you do start swimming again, it is important that you continue to exercise good hygiene around your stoma by rinsing with soap and clean water.
The Osseointegrated Prosthetic Limb (OPL) implant is compatible with a very wide variety of external prosthetic limb types.
Which one you choose will be determined by your prosthetist in line with your goals around safety and functionality.
Osseointegration, like any surgery, carries a degree of risk. Though shown to be a safe and effective therapeutic option, some patients may experience complications following their osseointegration surgery.
You can read more about potential complications, and how we minimise your risk, here.
Yes. It is possible to have the implant removed and return to use of a traditional socket-mounted prosthesis.